Radiotherapy Causes Genomic Changes in Breast Tumors

In many treatment plans for breast cancer, radiotherapy helps eliminate leftover cancer cells after clinicians remove the bulk of the tumor in surgery. While this method helps decrease cancer recurrence, researchers don’t know how radiotherapy induces changes in surviving tumor cells.1 Additionally, because of the postoperative use of radiotherapy, researchers have not been able to study its effect on the tumor microenvironment.
Simona Shaitelman explores the effects of radiotherapy and approaches to optimize its delivery.
University of Texas MD Anderson Cancer Center
“We were interested in looking at the effects of radiation on intact breast tumors to really try to understand the biological effects of radiation, and thus how to better optimize that treatment,” said Simona Shaitelmana physician scientist at the University of Texas MD Anderson Cancer Center.
To this end, in a Phase 2 clinical trialshe and her team reversed the order of standard breast cancer therapy: They delivered a single dose of radiation prior to surgical removal of patients’ tumors. Then, teaming up with cancer geneticist Nicholas Navin also at the University of Texas MD Anderson Cancer Center, they observed that radiotherapy alone caused genomic changes in the tumor and tumor microenvironment. The findings, published in Cell Reportscould help guide future trials for better cancer treatments.2
“The key strength of the paper is the fact that they’ve got a pure estrogen receptor positive breast cancer cohort of patients…and it has looked at the effect of radiation alone,” said Navita Somaiaha clinician scientist at The Institute of Cancer Research who also explores approaches to improve radiotherapy in breast cancer but was not involved with the study.
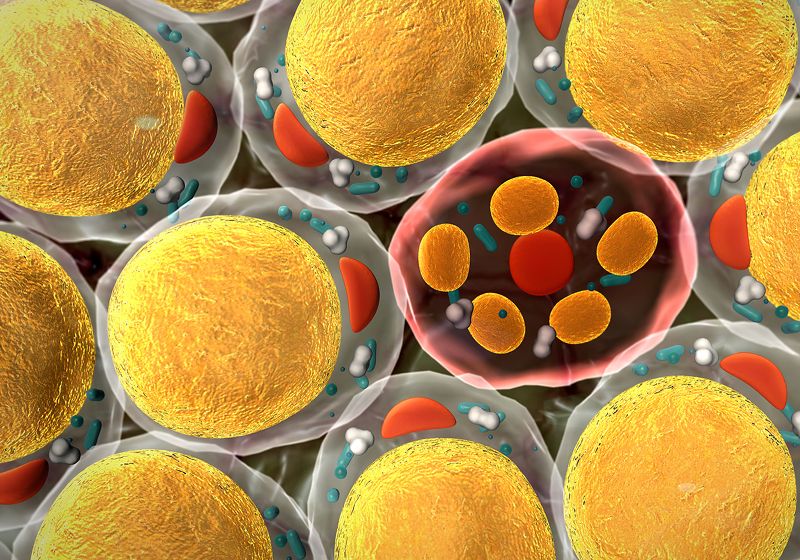
First, Shaitelman, Navin, and their team compared the gene expression of 11 patients’ tumors by single-cell RNA sequencing. They found that radiotherapy increased the number of macrophages, B cells, and CD4 T cells. They saw similar shifts across patients in populations of T cells, with increases in cell types associated with naive or memory populations and reduced numbers of most cytotoxic T cells. Meanwhile, macrophages had predominantly phagocytic and anti-tumor activity, though the type of T cell that they recruited differed between patients.
When they looked at the tumor cells’ response to radiotherapy, they saw an overall increase in genes related to stress response, and a decrease in genes related to interferon responses. Although radiation is known to cause DNA damage, the researchers did not see evidence of double-strand breaks or ongoing DNA damage repair.
Nicholas Navin develops novel technologies to cancer and cancer evolution at the genome level.
University of Texas MD Anderson Cancer Center
“We were expecting there to be a lot more DNA damage happening in the cancer cells,” Navin said. However, he said that this response may have already occurred and been resolved since they studied the tumors one week after the radiotherapy. Navin added that investigating the effect of higher radiation doses on DNA damage response pathways would be interesting in the future.
The team also found that radiotherapy did not affect the proliferation rate of tumor cells. Somaiah pointed out that this could be because the tumor populations studied are known to be less proliferative. “If you’re starting out with a very low proliferating population, you’re unlikely to pick up any differences in that population, so that’s why it’s not entirely surprising that they haven’t found anything like that,” she said.
They turned to single-cell DNA sequencing to study how radiotherapy changed tumor subclones, or cell populations within the tumor with distinct genomic mutations. While radiotherapy did not alter the number of subclones within the tumors, the team observed two distinct responses in patient tumors to radiotherapy.
In one group, radiotherapy altered the number of cells within these populations in some patients’ tumors. Cells in these tumors had higher expression of the gene encoding the estrogen receptor before and after radiotherapy and the androgen receptor after the treatment.
In contrast, in patients’ tumors where the populations within the subclones did not change with treatment, radiotherapy increased the numbers of immune cells and decreased the frequency of tumor cells. In this group, both the tumor and T cells had greater expression of checkpoint genes, which inhibit immune cell activity that can suppress tumor growth. Thus, patients with tumors that exhibit these signatures may not respond as well to radiotherapy or immune checkpoint blockade treatment.
Somaiah said that, despite the limited sample numbers and low radiation dose, the findings clearly point to effects of radiotherapy on tumors and the microenvironment. “What you start off with is not what you end with,” she said.
According to Shaitelman, these findings were intriguing because of clinical examples where patients with similar cancer profiles do not respond the same to therapy. “It lays a foundation of our moving the field forward to better customize and personalize how we will deliver radiation treatment to patients, and potential synergy with drugs that might modify radiation treatment as well,” she said.