First Use of Click Chemistry in Humans Safely Treats Cancer
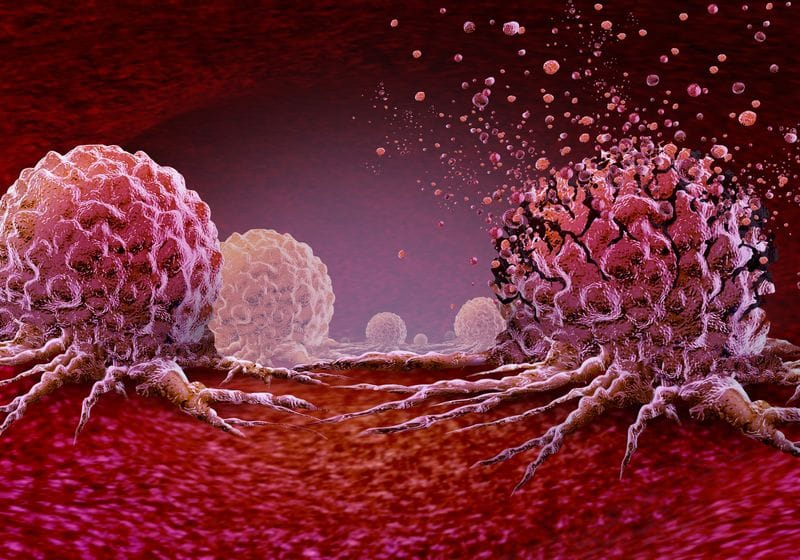
Chemotherapy, although lifesaving, causes a lot of side effects as it travels through the body to reach a cancerous tumor. From nausea to hair loss, these reactions arise because these drugs also inadvertently affect healthy cells.
José Mejía Oneto smiles and wears a blue collared shirt with his arms crossed.
Shasq
When he was an orthopedic surgery resident in 2012, José Mejía Onetowho is now the founder and chief executive officer of the biotech company Shasqwondered if he could develop cancer treatments that only act on tumor tissues, similar to how precisely he could replace a piece of bone with a metal implant. Incidentally, he came across an approach that he could use. Click chemistry, a technique where two chemicals ignore everything around them and only react when they come into contact and “click” together, had been developed about a decade prior.1
“Can we inject something that contains one of those new chemistry reagents, and then can we take a drug, modify it with the other click chemistry reagent, and then they’ll react with each other?” Oneto asked. “People had shown that there was a path that this could happen in vivo.”
Now, Oneto and his team at Shasqi have developed a click chemistry-based cancer drug that proved safe and evoked an anti-tumor immune response in both preclinical animal models and cancer patients in a small clinical trial.2 It is the first use of click chemistry in humans, setting the stage for the development of more targeted therapies based on this technology. They reported the results in Clinical Cancer Research.
“The fact that Shasqi has shown in this clinical trial that the chemistry works in humans—the components and the products are well tolerated in humans—I think that’s a pretty big benchmark, and I hope it goes all the way right to a therapeutic strategy to help patients,” said Stanford University biochemist Carolyn Bertozziwho shares a Nobel Prize for her research using click chemistry in living organisms and was not associated with the study. “But even in advance of that ultimate holy grail kind of milestone, I think this is still a big milestone.”
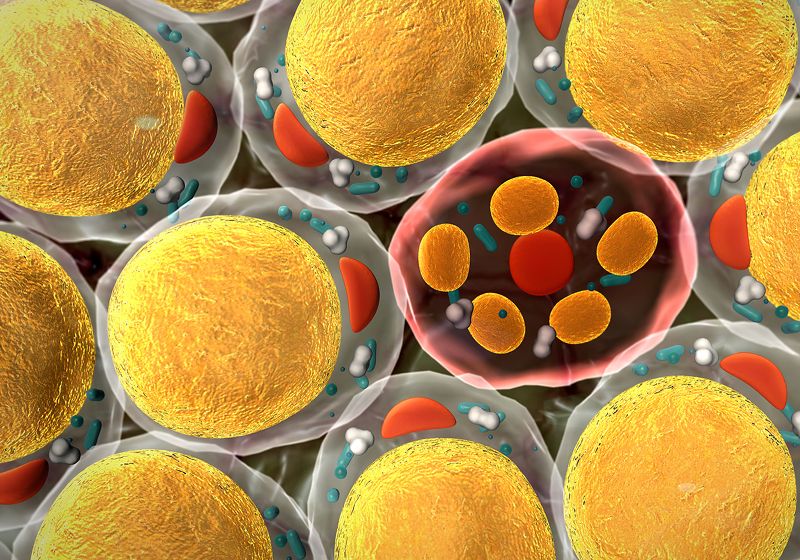
Shasqi’s drug, called SQ3370, consists of the two click chemistry components: tetrazine and trans-cyclooctene. One half of the drug contains tetrazine on a hyaluronic acid backbone. The researchers first inject the tetrazine-containing piece of the drug into the tumor. The second half of the drug carries the chemotherapy drug doxorubicin, which is inactive when bound to trans-cyclooctene. The team then delivers the trans-cyclooctene-bound doxorubicin half of the drug intravenously. When it reaches the tumor where the tetrazine is, trans-cyclooctene and tetrazine click together, releasing the now active doxorubicin drug precisely at the tumor.
“Doxorubicin is a very well-known drug. It has been around for 50, 60 years,” said Oneto. But, he added, “It’s highly toxic, and people can take about seven doses or so…in their lifetime, before they start running into cardiotoxicity.” Oneto and his team hoped that with a targeted approach, they could avoid some of doxorubicin’s adverse effects.
Carolyn Bertozzi won a Nobel Prize for her research using click chemistry in vivo. She developed biorthogonal chemical reactions that occur in cells without disrupting the cell’s biology.
American Chemical Society (ACS)
The team at Shasqi first tested how well SQ3370 worked in mouse models with different solid tumors, including melanoma, fibrosarcoma, and colorectal adenocarcinoma. They found that their drug slowed tumor progression and increased survival. The targeted therapy also recruited activated T cells at the tumor site, which led to a greater presence of anti-tumor immune cells there.
To evaluate the safety of the drug in a larger animal model, the Shasqi researchers injected the tetrazine piece of the drug into healthy dogs and then gave them an infusion of the trans-cyclooctene-doxorubicin part of the drug for five days in a row. They found that the drug was safe, the dogs tolerated it well, and the click chemistry worked, releasing the activated doxorubicin only in the location where they had injected the tetrazine component.
With the positive preclinical findings in mice and dogs, the team initiated a small Phase 1 clinical trial testing SQ3370 in people with advanced cancers, most of which were sarcomas, whose cancers had failed prior treatments.
“Our thought was, let’s go after soft tissue sarcomas. These are a rare type of tumor that is present often in the extremities and sometimes in the abdomen of patients, and usually you know where the location is of the initial site so that would allow you to do a direct injection to activate this doxorubicin,” said Oneto.
The researchers found that not only was SQ3370 safe and well-tolerated but, because they could target doxorubicin to the tumor so precisely, they could also deliver 15 times the normal dose of the drug without any cardiotoxicity. Consistent with their findings in the mouse models, the team also saw that SQ3370 induced a robust immune response in the tumor microenvironment in the patients.
While the therapy led to a median two to three months of disease stability in the patients in the trial, it was not as effective at halting cancer progression as the researchers had hoped. But, Oneto said, “This really opened up the door for us because it has taught us (that) it’s viable to do this approach, and then the question is, how do you make this approach be as helpful as possible to patients in the future?”
He and his team are exploring the ideas behind antibody-drug conjugates, for example, where they could target one piece of the drug to the tumor using an antibody and use click chemistry to activate it. In this case they wouldn’t have to inject one component of the drug and infuse the other, but they could infuse both, which would also have the benefit of making it easier for doctors to administer the drug.
David Bauerwho is a biomedical chemist at the University of Missouri and who was not involved in the current study but has collaborated with Shasqi in the past, agreed, adding that relying on injecting one piece of the drug into the tumor would limit the number of tumors this kind of drug could treat.
“A lot of cancer patients, most of them actually, will not be eligible for this study because if you have a solid tumor and it is resectable, you can get it out with surgery,” he said. But, he added, “Now we have the proof of concept that click chemistry really works in vivo.”
Both Bauer and Bertozzi are looking forward to what the team at Shasqi does next and how other groups will design new click chemistry-based drugs.
“To move the needle and to create something new, I think that has been the most rewarding path,” said Oneto. “The next level of rewards, I think, would be once we actually get drugs approved to patients, so that patients can use them and benefit from this technology. That is what I’m looking forward to in the future.”