Conjugate Vaccine Mechanisms, Design, and Immunological Memory
Plain capsular polysaccharide (CPS) vaccines against infectious diseases, introduced in the 1970s, elicit limited immune responses, particularly in children under two.1 In the 1980s, scientists overcame these limitations by pioneering CPS and protein conjugation, generating conjugate vaccines that trigger a robust immunologic responses.1,2 In this article, explore how scientists design conjugate vaccine technologies by converting polysaccharide antigens into T cell-dependent triggers that have revolutionized pediatric protection against encapsulated bacteria and other pathogens.
Conjugate vaccine efficacy is characterized by a robust immune response involving memory cells and plasma cell production of high affinity antibodies.
istock, self
How Conjugate Vaccines Rewire Immune Recognition
Conjugate vaccines are composed of bacterial polysaccharide antigens covalently linked to protein carriers, enabling T cell-dependent immune responses that induce high-affinity antibodies and immunological memory.3,4 Common examples include the Haemophilus influenzae type b (Hib) vaccine, pneumococcal conjugate vaccines, and meningococcal conjugate vaccines, which help protect against bacterial infections that cause meningitis and pneumonia, among other infectious diseases.
Conjugate Vaccine T Cell Engagement Mechanisms
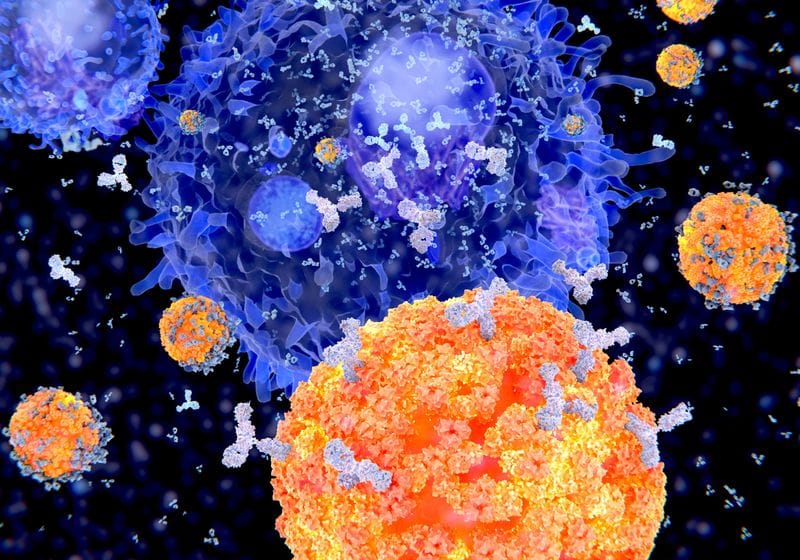
Researchers developed conjugate vaccines by covalently linking the CPS to a protein carrier, creating an immunogenic conjugate also called a glycoconjugate.1,3 For example, Hib conjugate vaccines are commonly made out of the Hib bacterium’s polysaccharide capsule and modified proteins isolated from other bacteria. Unlike CPS-only vaccines that are not processed for antigen presentation by a B cell’s major histocompatibility complex class II molecules (MHCII), membrane-bound B cell receptors bind to the polysaccharide component of the conjugate vaccine, internalize the entire conjugate, and processes it for antigen presentation to T cells.3
MHCII presentation by B cells enables a T cell-dependent response, which provides co-stimulation and cytokine support that drives B cell proliferation, germinal center formation, and isotype switching.3,6 As a result, the B cell undergoes affinity maturation, producing high-avidity IgG antibodies and forming long-lived plasma and memory B cells.1,6
B cells that recognize polysaccharide-only antigens mount a limited T cell-independent immune response that generates short-lived plasma cells and low-affinity antibodies without memory formation. Conjugate vaccines enable B cells to internalize and present carrier-derived peptide or glycopeptide antigens to T cells, which support B cell differentiation, affinity maturation, and immune memory.
modified from © istock.com, Pikovit44, Wooden, TTSZ, ClusterX; designed by erin lemieux
Carrier Proteins and Conjugate Vaccine Design
Conjugate vaccine immunogenicity depends on the quality and number of distinct polysaccharides and the selected carrier protein.7 Scientists select carrier proteins to support vaccine efficacy based on the carrier’s ability to do the following.2,8
- Induce strong helper T cell responses
- Minimize interference with other vaccines, called carrier-induced epitope suppression (CIES)
- Tolerate the addition of multiple different polysaccharides
Recent studies suggest that some CD4+ T cells may directly recognize glycopeptide fragments, or carbohydrates, not just carrier protein peptides. Researchers postulated that carbohydrate-specific CD4+ helper T cells (Tcarb) may recognize portions of the polysaccharide chain that remain bound to the carrier protein’s peptides after processing and thus are part of the MHCII molecules’ presentation.1,6 This means that different conjugate vaccines may engage distinct peptide or glycopeptide antigen presentations, highlighting T cell response diversity.6
A carrier protein’s ability to function across different production platforms is also important. Some carriers are more compatible with modern bioengineering approaches used in recombinant or cell-free manufacturing.8-10
Conjugate Vaccine Manufacturing and Bioengineering Platforms
Modern manufacturing platforms allow precise and scalable construction of glycoconjugates.
Traditional conjugate vaccine production involves isolating capsular polysaccharides from pathogens and chemically linking them to carrier proteins.8 This multi-step process requires extensive purification to remove endotoxins and verify conjugate integrity.8 While effective, these methods are costly, susceptible to batch variability, and difficult to scale.8,9
To meet global demand and lower costs, researchers use bioengineering to simplify glycoconjugate production. Bioprocessing platforms such as Protein Glycan Coupling Technology (PGCT) simplify production by enabling recombinant glycoconjugate expression in engineered E. coli.8,9 This approach involves transfecting bacteria with three key plasmids that encode the following.9
- The carrier protein expressing a glycosylation motif
- Bacterial polysaccharide biosynthesis
- An oligosaccharyltransferase enzyme (typically C. jejuni PglB), which catalyzes the transfer of the assembled glycan onto the carrier protein
Cell-free or synthetic systems such as the in vitro conjugate vaccine expression (iVAX) platform offer key advantages: they are thermostable for ambient storage, compatible with multiple carrier-glycan pairs, minimize endotoxin content, and support scalable, portable production.11 Researchers designed the iVAX platform so that clinicians can rehydrate freeze-dried lysates at the point of care to generate clinically relevant doses of conjugate vaccine within an hour.11
Clinical Applications and Ongoing Challenges
Conjugate vaccine dosing schedules vary by recipient age and are critical in shaping the quality of the immune response.3 When administered early in life, conjugate vaccines prime the immune system to generate memory B cells that mount robust secondary responses upon subsequent exposure or booster vaccinations.3 These memory responses can persist for years, forming the basis for long-term protection.2 The timing of booster doses influences memory B cell output magnitude and durability, particularly in young children whose germinal center responses continue to mature after initial priming.3
Beyond individual protection, conjugate vaccines reduce nasopharyngeal colonization of targeted bacteria, limiting transmission and contributing to herd immunity.2,7 Researchers have documented herd immunity effects across Haemophilus influenzae, Streptococcus pneumoniaeand Neisseria meningitidiswith substantially reduced transmission lowering disease incidence in both vaccinated and unvaccinated populations.2
The repeated use of the same carrier protein across multiple vaccines can reduce the immune response to newly introduced polysaccharide components—a phenomenon known as carrier-induced epitope suppression. This challenge has prompted interest in developing novel or alternating carriers to sustain vaccine efficacy across increasingly complex immunization schedules.2,4
Future Directions
Conjugate vaccines remain a cornerstone of modern vaccinology due to their ability to elicit robust, durable, and protective immune responses across age groups.3 This mechanism transforms a poorly immunogenic polysaccharide into a highly immunogenic antigen capable of inducing durable protective immunity.3 Ongoing mechanistic insights, particularly into antigen presentation pathways, alternative carrier agents, and age-specific immune dynamics, will continue to inform improvement in vaccine design and deployment strategies.4
- Rappuoli R, et al. On the mechanisms of conjugate vaccines. Proc Natl Acad of Sci U S A. 2019;116(1):14–16.
- Pichichero me. Protein carriers of conjugate vaccines: Characteristics, development, and clinical trials.Hum Vaccin Immunother. 2013;9(12):2505–23.
- Rappuoli R. Glycoconjugate vaccines: Principles and mechanisms. Sci Trans Med. 2018; 10 (456): Eatuz416.
- van der put rmf, et al. Carriers and antigens: New developments in glycoconjugate vaccines. Vaccines (Basel). 2023;11(2):219.
- Goldblatt D. Conjugate vaccines. Clin Exp Immunol. 2000;119(1):1–3.
- Sun X, et al. Polysaccharide structure dictates mechanism of adaptive immune response to glycoconjugate vaccines. Proc Natl Acad Sci U S A. 2019;116(1):193–198.
- POLLARD AJ, et al. Maintaining protection against invasive bacteria with protein-polysaccharide conjugate vaccines.Nat Rev Immunol. 2009;9(3):213–20.
- Kay e, et al. Recent advances in the production of recombinant glycoconjugate vaccines. NPJ Vaccines. 2019;4(1):1–8.
- Cuccu J et al. Exploitation of bacterial N-linked glycosylation to develop a novel recombinant glycoconjugate vaccine against Francisella tularensis. Open Biol. 2013;3(5):130002.
- Stark JC, et al. On-demand biomanufacturing of protective conjugate vaccines. Sci Adv. 2021; 7 (6): Eabe9444.
- Warfel KF, et al. A low-cost, thermostable, cell-free protein synthesis platform for on-demand production of conjugate vaccines. ACS Synth Biol. 2023:12(1):95-107.