A Selective Protein Regulates Chronic, But Not Acute, Inflammation New
Estimated reading time: 4 minutes
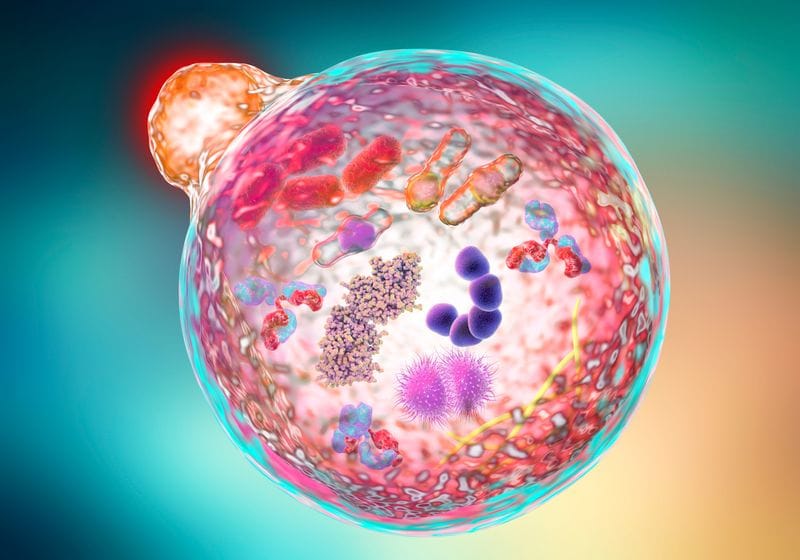
Researchers at Massachusetts General Hospital identified a novel nuclear autophagy-based mechanism that distinguishes chronic inflammation from its acute counterpart.
Anyone who’s ever scraped their knee on a dirty playground is familiar with the stinging inflammation that manifests soon after the injury. It’s the immune system’s effort to restrict and neutralize any foreign pathogens that might have entered the body. While acute inflammation subsides after the infection passes, chronic inflammation can last for a long time and worsen disease progression. In fact, such persistent inflammation can lead to cardiovascular disease, diabetes mellitus, non-alcoholic fatty liver disease, and autoimmune and neurodegenerative disorders.1
“Inflammation is a double-edged sword,” said Zhixun Doua regenerative biologist at Massachusetts General Hospital. “Against infection, it’s good. But chronic inflammation, which is often in the absence of infection, is problematic.” As of 2019, more than 50 percent of global deaths can be attributed to chronic inflammatory diseases.1 Yet there’s a dire lack of targeted therapies that treat chronic conditions without blunting beneficial acute inflammation. In a recent study published in NatureDou and his team identified a new protein that specifically regulates chronic inflammation, leaving acute inflammation unperturbed.2 Their findings could pave the way for improved therapies for chronic inflammatory diseases.
“It’s really interesting because the major challenge of chronic inflammation is how to find strong markers that could be targets of therapies,” said Aurelia Santoroa molecular biologist at the University of Bologna who studies aging and inflammation and was not involved in the study. “These findings point toward future precision anti-inflammatory therapy that’s needed to counteract chronic diseases.”
Studying the nitty-gritty of how acute and chronic inflammation differ was not on Dou’s radar. His group studies aging and age-associated diseases, both of which are characterized by systemic chronic inflammation. At the onset of one project, Dou wanted to identify proteins that cells lose as they becomes senescent; he was particularly focused on those targeted by nuclear autophagy—a process by which cells remove damaged or dysfunctional nuclear components to maintain homeostasis.3
Using human skin cells, the team first performed an assay to pull out the binding partners of autophagy mediators and observed strong enrichment of chromatin-remodeling proteins that affect gene expression and silencing. To determine which of these were crucial to aging, the researchers analyzed the nuclear proteomes of senescent skin cells and young cells. They observed that aged cells lost a subset of chromatin-remodeling proteins. Upon comparing the candidates to the previously identified autophagy targets, they converged on a protein called Williams syndrome transcription factor (WSTF) and hypothesized that its loss drives cellular aging.
WSTF changes the chromatin state from open to closed, consequently repressing the expression of the targeted genes.4 To determine how it regulates aging, Dou and his team overexpressed WSTF in human skin cells. While they observed minimal impact on markers of senescence, the manipulation impaired age-associated inflammation. Disrupting WSTF’s function enhanced inflammation. This serendipitous finding changed the course of the study.
Dou then wondered what happens to WSTF in acute inflammation. “To our great, great surprise, this process was not involved in acute inflammation,” he exclaimed. The team injected bacterial sugar molecules into human skin cells to induce acute inflammation and observed no impact on the levels of WSTF.
To further understand the mechanism by which WSTF regulated chronic inflammation, the study authors inhibited its binding to nuclear autophagic proteins. Though manipulation reduced the expression of chronic inflammatory markers, it had no effect on those of acute inflammation.
“This is probably the first time that we can mechanistically separate chronic from acute inflammation,” Dou said.
Dou and his team then investigated the levels of WSTF in other conditions, such as chronic inflammation of the liver and joints. They analyzed samples of diseased human liver and cartilage and observed reduced levels of WSTF in the nuclei. To explore if WSTF could be a therapeutic target, the team created mouse models of chronic liver inflammation and osteoarthritis and injected the animals with a molecule that blocked binding between WSTF and nuclear autophagy proteins. The treatment attenuated the inflammation in the tissues, reduced liver fibrosis, and lessened cartilage damage in the joints.
Going forward, Duo wants to explore the role of WSTF in other chronic diseases and screen for more proteins that might play a role in the regulation of aging and inflammation.




